The efficacy of BRUKINSA®▼ for the treatment of chronic lymphocytic leukaemia (CLL) was evaluated in two randomised controlled phase 3 studies; one involving patients with previously untreated CLL, and the other involving patients with relapsed/refractory (R/R) CLL.1–6 Additionally, long-term data have been generated from extended follow-up of the phase 3 ALPINE study.6
SEQUOIA was a phase 3, open-label, randomised study, comparing BRUKINSA with bendamustine + rituximab (BR) in patients with previously untreated CLL.2,3
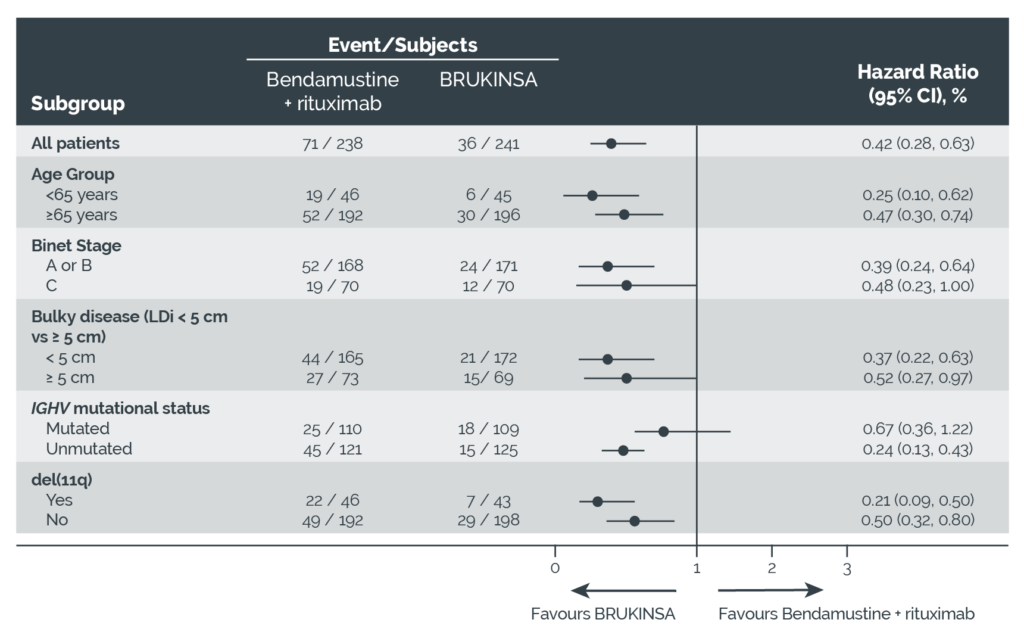
ALPINE was a phase 3, open-label, randomised, multicentre, head-to-head study comparing BRUKINSA with ibrutinib in patients with R/R CLL.4–6
Learn more about the SEQUOIA and ALPINE studies
BRUKINSA demonstrated significantly improved progression-free survival (PFS) versus BR in the SEQUOIA study, and significantly superior overall response rate (ORR) versus ibrutinib in the ALPINE study.2–5
- SEQUOIA study
- ALPINE study
- ALPINE study: Extended follow-up
Efficacy in the SEQUOIA study
Progression-free survival (PFS)
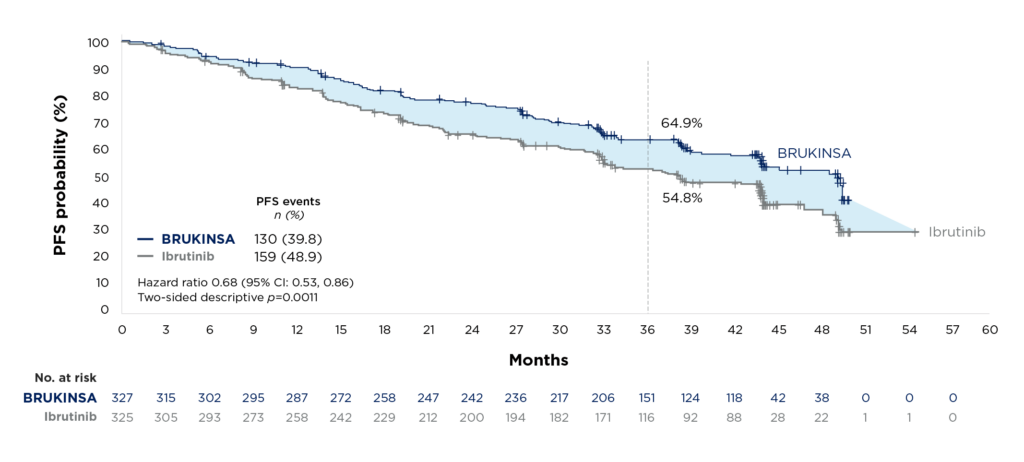
In the SEQUOIA study, independent review committee (IRC)-assessed PFS in Cohort 1 (patients without del[17p]) was the primary endpoint, and this was met at the interim analysis.1,2 PFS was longer with BRUKINSA compared with BR (Figure 1).1,2
At 24 months, the estimated PFS rate in Cohort 1 was 85.5% (95% confidence interval [CI]: 80.1, 89.6) for BRUKINSA versus 69.5% (95% CI: 62.4, 75.5) for BR.1,2 After a median follow up of 26.2 months, the IRC determined that PFS was significantly improved with BRUKINSA versus BR (hazard ratio 0.42 [95% CI: 0.28, 0.63]; two-sided p<0.0001; Figure 1).1,2
Figure 1. SEQUOIA: Kaplan-Meier estimates of IRC-assessed PFS for Cohort 1 (patients without del[17p]).2
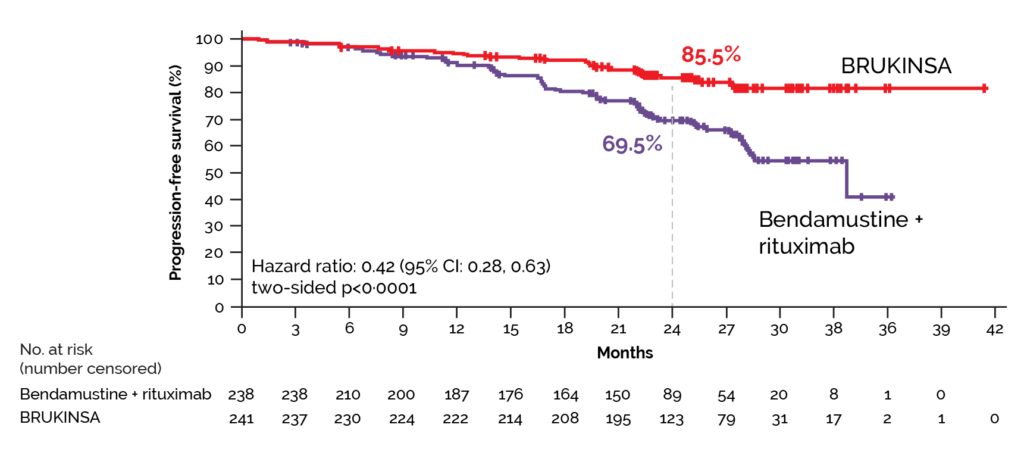
In Cohort 1, PFS was consistently longer with BRUKINSA compared with BR across almost all prespecified subgroup analyses, including patients with baseline high-risk disease status (Figure 2).2
Figure 2. SEQUOIA: IRC-assessed PFS across subgroups for BRUKINSA versus BR in Cohort 1 (patients without del[17p]).2
Consistent results were observed between IRC-assessed PFS and investigator-assessed (IA) PFS, which was a key secondary endpoint in the SEQUOIA study.2 An updated analysis was conducted after a median follow-up of 43.7 months for Cohort 1.3 Median IA-PFS was not reached in the BRUKINSA group compared with 42.2 months in the BR group.3 Estimated 42-month PFS rates were 82.4% for BRUKINSA and 50.0% for BR.3 IA-PFS was significantly improved with BRUKINSA versus BR with mutated IGHV (2-sided p=0.00033) and unmutated IGHV (2-sided p=0.0001).3
Cohort 2 of the SEQUOIA study included patients with del(17p).2 After a median follow-up of 30.5 months (interquartile range 27.6–33.1), median IRC-assessed PFS was not reached.2 The estimated PFS rate at 24 months was 88.9% (95% CI: 81.3, 93.6).2 After a median follow-up of 47.9 months, median IA-PFS in Cohort 2 was not reached and the estimated 42-month PFS rate was 79.4%.3
Overall response rate (ORR)
In Cohort 1 (patients without del[17p]), IRC-assessed ORR, was 94.6% (228/241; 95% CI: 91.0, 97.1) in the BRUKINSA group, and 85.3% (203/238; 95% CI: 80.1, 89.6) in the BR group.2 In the BRUKINSA group, 16 (7%) of 241 patients had a complete response, as assessed by IRC, versus 36 (15%) of 238 patients in the BR group.2 For Cohort 2 (patients with del[17p]), IRC-assessed ORR was 90.0% (99/110; 95% CI: 82.8–94.9).1,2